Characterization of H type 1 and type 1 N-acetyllactosamine glycan epitopes on ovarian cancer specifically recognized by the anti-glycan monoclonal antibody mAb-A4.
Choo, M; Tan, HL; Ding, V; Castangia, R; Belgacem, O; Liau, B; Hartley-Tassell, L; Haslam, SM; Dell, A; Choo, A
J Biol Chem
292
6163-6176
2017
Show Abstract
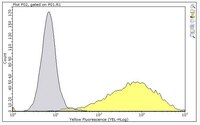
Cancer-specific glycans of ovarian cancer are promising epitopes for targeting with monoclonal antibodies (mAb). Despite their potential, structural characterization of these glycan epitopes remains a significant challenge in mAb preclinical development. Our group generated the monoclonal antibody mAb-A4 against human embryonic stem cells (hESC), which also bound specifically to N-glycans present on 11 of 19 ovarian cancer (OC) and 8 of 14 breast cancer cell lines tested. Normal cell lines and tissue were unstained by mAb-A4. To characterize the N-linked glycan epitopes on OC cell lines targeted by mAb-A4, we used glycosidases, glycan microarray, siRNA, and advanced high sensitivity matrix-assisted laser desorption/ionization mass spectrometry (MALDI-MS). The mAb-A4 epitopes were found to be Fucα1-2Galβ1-3GlcNAcβ (H type 1) and Galβ1-3GlcNAcβ (type 1 LacNAc). These structures were found to be present on multiple proteins from hESC and OC. Importantly, endo-β-galactosidase coupled with MALDI-MS allowed these two epitopes, for the first time, to be directly identified on the polylactosamines of N-glycans of SKOV3, IGROV1, OV90, and OVCA433. Furthermore, siRNA knockdown of B3GALT5 expression in SKOV3 demonstrated that mAb-A4 binding was dependent on B3GALT5, providing orthogonal evidence of the epitopes' structures. The recognition of oncofetal H type 1 and type 1 LacNAc on OC by mAb-A4 is a novel and promising way to target OC and supports the theory that cancer can acquire stem-like phenotypes. We propose that the orthogonal framework used in this work could be the basis for advancing anti-glycan mAb characterization. | 28167527
 |
Inhibition of TRF1 Telomere Protein Impairs Tumor Initiation and Progression in Glioblastoma Mouse Models and Patient-Derived Xenografts.
Bejarano, L; Schuhmacher, AJ; Méndez, M; Megías, D; Blanco-Aparicio, C; Martínez, S; Pastor, J; Squatrito, M; Blasco, MA
Cancer Cell
32
590-607.e4
2017
Show Abstract
Glioblastoma multiforme (GBM) is a deadly and common brain tumor. Poor prognosis is linked to high proliferation and cell heterogeneity, including glioma stem cells (GSCs). Telomere genes are frequently mutated. The telomere binding protein TRF1 is essential for telomere protection, and for adult and pluripotent stem cells. Here, we find TRF1 upregulation in mouse and human GBM. Brain-specific Trf1 genetic deletion in GBM mouse models inhibited GBM initiation and progression, increasing survival. Trf1 deletion increased telomeric DNA damage and reduced proliferation and stemness. TRF1 chemical inhibitors mimicked these effects in human GBM cells and also blocked tumor sphere formation and tumor growth in xenografts from patient-derived primary GSCs. Thus, targeting telomeres throughout TRF1 inhibition is an effective therapeutic strategy for GBM. | 29101385
 |